3 Steps to Prevent Body Shaming at Your Child’s Next Well-Check Visit
I remember the first time I figured out that our pediatrician’s office could be a minefield of triggers for food and body shame.
Honestly, it shouldn’t have surprised me - given how weight-centric our healthcare system is here in the United States.
And perhaps, I’m more hypersensitive to it as a mom in eating disorder recovery, as I clearly remember the comments doctors made to me about my own body at various appointments in my growing up.
But I didn’t expect it to surface as soon as it did.
Like when our pediatrician told me that I “really should lay off the sweets and snacks” for my daughter because my 2 year old was off the growth charts. Or when I was questioned if I was feeding my 5 year old because he was in a thinner body. (Mind you - they were both maintaining their individual growth trajectories on their growth charts, even though one happens to be in a larger body and one in a smaller body).
Even as a dietitian mom who understands that growth charts are not indicators of my children’s overall health, I felt shame and judgment at my kids’ check-ups.
It made me aware how commonplace this is for a majority of parents who are doing their best to navigate a fat phobic healthcare system, and who are trying to make sense of growth charts - often with little explanation from the providers who are seeing them.
On top of which, parents are often thrown shade about how they feed and care for their children, with judgements made simply based on where your child’s plot points fall on their growth charts. Like how our provider assumed I was giving my daughter free rein of all the sweets and snacks in our house or that I wasn’t feeding my son, simply because of their body sizes.
It’s all too easy to internalize these types of food and body shaming comments from healthcare providers as personal failure on our parts as parents.
This can make parents feel inadequate, stop seeking out healthcare altogether, or begin to engage in harmful feeding practices that can put their kids at risk for eating disorders (like restricting their overall caloric intake because a doctor recommended weight loss or pressure a child to eat foods they may not be ready to eat).
But perhaps the most dangerous of all is the risk these types of body and food shaming comments from health care providers have on our children and their relationships with food and their bodies.
Studies have found that body shame has the strongest relationship to eating problems, with body shaming to present as one of the strongest eating disorder risk factors in children.
These risks are even higher in children who have a history of eating disorders in their families. So if you have had an eating disorder or are currently in eating disorder recovery, this is even more important for you to pay attention to to help lower your child’s risk.
What’s important to understand is that even if your provider has good intentions, poor delivery around food and body image concerns can be construed as body shaming for kids. All it takes is one comment for kids to latch on to that could trigger harmful thoughts and behaviors around food and body.
Especially in light of the pandemic, weight stigma in the healthcare industry, and hyperfocus on ob*sity “prevention efforts”, our kids are more at risk for eating disorders than ever, with incidences of hospitalizations and treatment for pediatric eating disorders surging since the onset of the pandemic
Thankfully, even the American Academy of Pediatrics (AAP) has woken up to the real risks of eating disorders and associated body shaming, creating a position policy where they outline specific guidelines for pediatricians in effort to curb how weight is typically addressed in well-check visits.
From the AAP clinical report in 2016 titled, “Preventing Obesity and Eating Disorders in Adolescents”, it notes the following information: (Bolding added for emphasis)
“There are concerns that obesity prevention efforts may lead to the development of an [eating disorder]. Most adolescents who develop an ED did not have obesity previously, but some teenagers, in an attempt to lose weight, may develop an ED.”
And…
“Most adolescents who develop an ED did not have obesity previously, but some adolescents may misinterpret what “healthy eating” is and engage in unhealthy behaviors, such as skipping meals or using fad diets in an attempt to “be healthier,” the result of which could be the development of an ED. Messages from pediatricians addressing obesity and reviewing constructive ways to manage weight can be safely and supportively incorporated into health care visits. Avoiding certain weight-based language and using motivational interviewing (MI) techniques may improve communication and promote successful outcomes when providing weight-management counseling.”
Even with these updated guidelines from the AAP recommending that pediatricians skip the weight talk in your child’s well-check visits, I can tell you that these guidelines are far from being implemented as part of standardized pediatric care.
This means as a parent, you often have to take matters into your own hands to protect your child’s health and well-being, and to prevent the occurence of body shaming as their next well-check visit.
As mentioned earlier and worth noting again, this is even more important if you yourself have an eating disorder, have struggled with an eating disorder in the past, or have any history of an eating disorder in your family.
Because eating disorders have a strong genetic component, your child will have a higher risk of developing an eating disorder. This does NOT mean your child is automatically guaranteed to have an eating disorder or that your struggle will also become theirs.
It simply means they are at elevated risk compared to a child who has no family history of eating disorders. It also means you CAN help decrease your child’s risk of developing an eating disorder by lowering risk factors wherever possible - starting with the doctor’s office.
Again, you wouldn’t expect a routine well-check for your child to be a place for weight/body-shaming comments.
Sadly, it happens more often than you think.
With growth charts at the front and center of your child’s appointment, your provider might remark on your child’s weight, body size or eating habits.
Your doctor may misdiagnose your child based on their body size and BMI, labeling them as “ob*se”, making misjudgements about how or what you feed them. (And just to be clear, this happens on both sides of the spectrum. Children in both larger and smaller bodies may be mistyped, misjudged, and miscategorized based on where their body size lands).
These types of comments can trigger food and body image issues, which could haunt your child for years to come, especially if there is a family history of eating disorders.
3 Steps to Prevent Body Shaming at Your Child’s Well-Check Visit
Thankfully, there are some proactive things you can do to help prevent these things from happening.
Consider this step by step approach below to help you navigate this:
1. Connect with your provider:
If possible, before your child’s next well-check visit, take the time to contact your provider.
Depending on the type of system you’re in, you may or may not be able to make direct contact with your provider, though it can be helpful to make the attempt.
If you’re unsure how to get in touch with your provider, call the office directly and ask what is the best way to relay a concern to your child’s doctor ahead of your visit.
2. Communicate your requests:
You want to communicate with your provider specifically that you do not want any discussion of your child’s weight, growth charts or diets in front of your child, or while your child is present during the appointment.
Also request that your provider address any concerns about your child’s weight/growth with you privately, without your child present.
If your child has previously shown distress around being weighed, you can also request that blind weights are conducted for your child’s appointment (where your child is weighed without seeing the number).
These requests can be relayed to your provider ahead of time via your doctor’s electronic messaging system, through a phone call or by leaving a voicemail, depending on your doctor’s office.
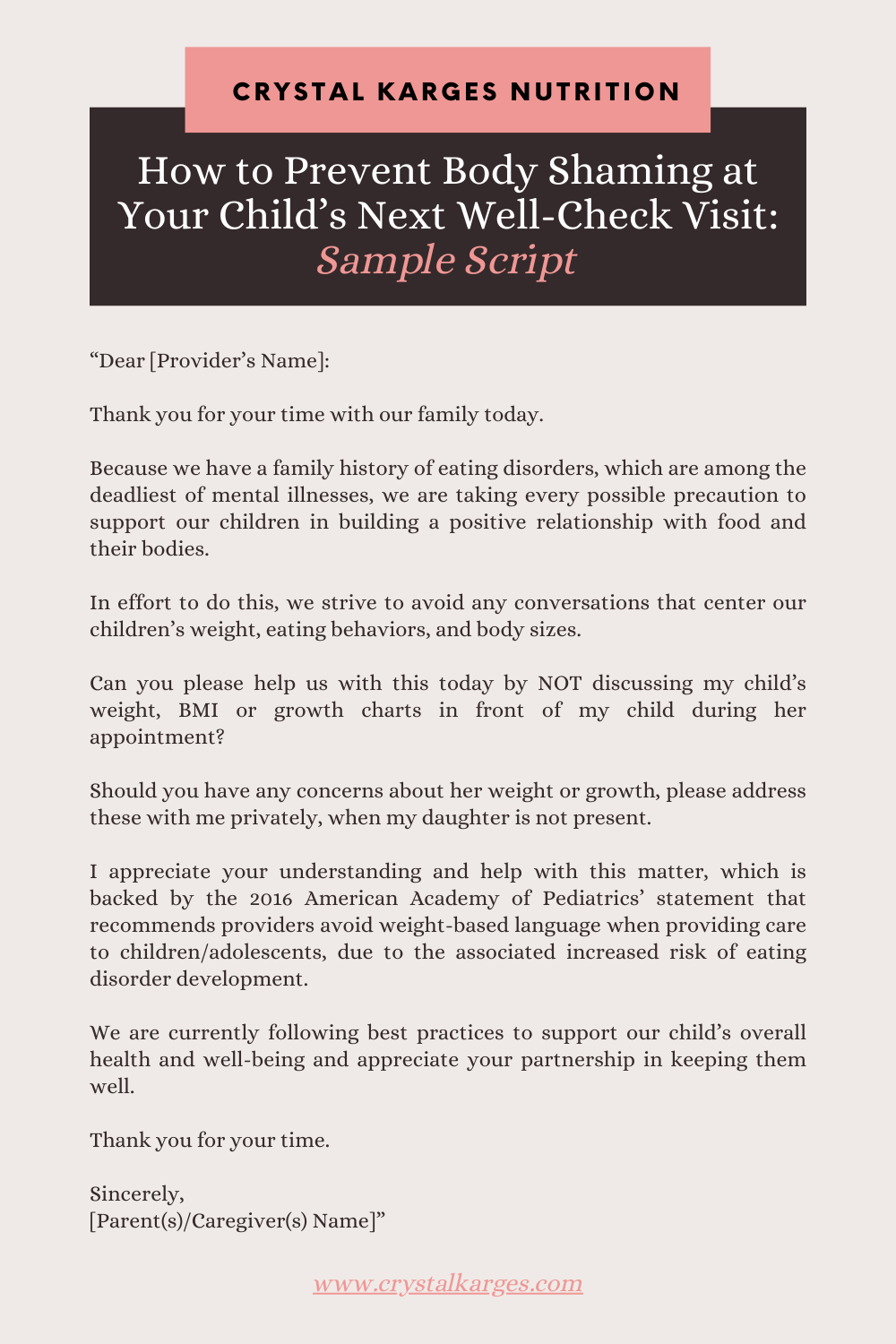
3. Capture your requests in a written letter:
In addition, consider writing out a letter to bring with you to your child’s appointment. Even if you made contact with your provider, I still recommend bringing a typed letter with your requests to hand to your doctor at the actual appointment.
A sample script could look like this:
“Dear [Provider’s Name]:
Thank you for your time with our family today.
Because we have a family history of eating disorders, which are among the deadliest of mental illnesses, we are taking every possible precaution to support our children in building a positive relationship with food and their bodies.
In effort to do this, we strive to avoid any conversations that center our children’s weight, eating behaviors, and body sizes.
Can you please help us with this today by NOT discussing my child’s weight, BMI or growth charts in front of my child during her appointment?
Should you have any concerns about her weight or growth, please address these with me privately, when my daughter is not present.
I appreciate your understanding and help with this matter, which is backed by the 2016 American Academy of Pediatrics’ statement that recommends providers avoid weight-based language when providing care to children/adolescents, due to the associated increased risk of eating disorder development.
We are currently following best practices to support our child’s overall health and well-being and appreciate your partnership in keeping them well.
Thank you for your time.
Sincerely,
[Parent(s)/Caregiver(s) Name]”
From my experience, it has required multiple attempts to connect with my provider.
Sometimes, my kids will be assigned to a different pediatrician at each appointment, so even while I may’ve made this request with a previous provider, this doesn’t necessarily mean there is a mutual understanding of your requests.
This is why, no matter what, I’ll always bring a typed-out letter with me to hand directly to our doctor when they first come into the office with my child.
I don’t want to assume they know, even if I’ve made the effort to contact them or leave a message. I understand pediatricians are seeing multiple patients a day, and I don’t expect them to remember me and my request.
To err on the side of caution, I would also recommend making the effort to reach out ahead of time AND also bring your typed letter with you as well. In this way, you’re covering all your bases to ensure your doctor understands your position and requests.
I also have found letters to be more straightforward (not a whole lot of room for misinterpretation). This can also be a helpful means of communication if you’re worried about how/what to say to your provider.
Advocating for Your Child’s Wellbeing
It can be scary to speak up and advocate for your child, especially if you hold a marginalized identity or have a history of medical trauma.
Please know your voice and concerns matter.
You know your child best, and your advocacy efforts will not go in vain.
It’s possible to enlist the support of other caregivers and providers to advocate for your child too if you don’t have the capacity to do so. Writing a letter ahead of time can also help you clearly articulate your thoughts and requests without having to do so on the spot during the appointment.
You can download a free template below that you can use to customize for you and your child before your next appointment. You don’t have to do this alone.
Growth Charts Aren’t an Indicator of Your Child’s Health
Hearing and seeing numbers around BMI, weight and growth chart are not only confusing to kids but to their parents, too. There’a a chance your doctor may speak with you privately about your child’s weight and body size, or have questions about how you’re feeding them.
These can be hard conversations to have, even if your pediatrician is not addressing these matters in front of your child.
One helpful thing to remember is that growth charts and weight status are NOT a good indicator of your child’s overall health and well-being.
Unfortunately, some clinicians do make faulty assumptions about children and how they are taken care of based on their numbers, which is unethical and unfounded.
This is where you need to keep the big picture in mind when it comes to your child’s overall health.
Health is not determined by a size, by BMI or by a number on the scale. There are multiple determinants of health, including our genetics, environment, social circumstances, sleep, movement, and mental health - all which are crucial for determining our overall health.
The same is true for your kids.
Some providers might make recommendations for weight loss based for your child based on where they fall on the growth chart - and this is NOT best practice for supporting a child’s health.
It may seem counterintuitive to everything our culture tells us makes us “healthy”; though you have to remember, our culture is largely saturated by a multi-billion dollar dieting industry, if that tells you anything about what oppressive systems are upheld in our society.
Studies have shown that dieting in children is the NUMBER ONE PREDICTOR of new eating disorder development, and remember, this risk is elevated in children with a family history of eating disorders. [Include stat link]
For these reasons, you can strongly decline any such recommendations from a provider and insist you are focusing on your child’s health as a whole, doing everything possible to avoid their eating disorder risk.
For more ways on how to support your child’s health without dieting, be sure to check out this blog post here for more ideas: “Instead of a Diet for Kids, These Healthy Habits Create Real Change”
And REMEMBER: Growth charts are NOT a good indicator of your child’s health.
Everything you’re doing matters to your child and ensuring they have the best shot possible and growing into their healthiest selves while building a positive relationship with food and their bodies.
What has been your experience with well-check visits?